Content Warning: This article contains references to disordered eating and mental health issues that may be upsetting for some readers.
In a monologue in 2019, the talk show host Bill Maher used his show, “Real Time,” as a platform to address the rise of obesity in the United States. “In August, 53 Americans died from mass shootings. Terrible, right?” he said. “Do you know how many died from obesity? 40,000.”
“Fat shaming doesn’t need to end,” Maher added. “It needs to make a comeback.”
Fat shaming, and body shaming in general, remains a highly prevalent phenomenon. Even medical professionals have been shown to engage in such behavior: roughly 3 in 5 adults with obesity experience weight bias in medical environments, according to Obesity Canada. In the meantime, obesity has been on the rise in many countries. More than 40% of American adults are classified as obese (a Body Mass Index (BMI) over 30), according to the Centers for Disease Control and Prevention (CDC). In the face of these rising rates, many people feel compelled to confront peers over their weight and eating, often with the genuine, selfless motive of encouraging better health. However, attempting to pressure people into losing weight is more likely to encourage unhealthy behaviors.
Many Americans use dieting to maintain good health, including parents, according to Tessa Komine, a Registered Dietician Nutritionist (RDN) who specializes in treating eating disorders, and children learn to think the same way their parents do. “They observed watching their parents struggle with body image and watching them, you know, label food in a certain way or restrict food themselves,” says Komine. Many children internalize those perceptions, and body image issues can begin from a young age.
I was one of those children. By fourth grade, my weight had become an obsession. In every mirror I evaluated how my weight had changed that day. When I didn’t see what I wanted, a pit grew in my stomach. I began to eat so I could numb my feelings of shame. And that shame compelled me to hide what I was doing. Whenever I could hear a parent or my brother approaching as I ate, I hurried out of the room so that no one could see what I was doing. I didn’t eat any less; I just hid how much I was eating.
Binge-eating, or eating heavily and out of proportion to someone’s hunger, is one of the most common responses to body shaming. According to the Canadian Medical Association Journal (CMAJ), experiences with weight bias trigger stress responses in people, producing the stress hormone cortisol. Many cope with this stress through excessive eating. The result is a vicious cycle of weight gain and mental health issues.
Another common response to fat shaming is to avoid treatment for fear of being shamed or ignored due to weight issues. Just one in 10 people who experience eating disorders receive treatment, according to the South Carolina Department of Mental Health (SCDMH). “I have lots of clients who […] are afraid to go to the doctor because […] being in a larger size in a larger body, they fear judgment from their providers,” says Komine. I myself have trouble going to the doctor’s office. When my appointment begins, I am taken to a scale almost immediately, and the idea of having my weight measured terrifies me.
At times my parents would comment on my weight. Their feedback stung, making me want to change my habits. I cut out carbohydrates, dairy, sugar, anything I believed would make me overweight. At the same time, I was involved in Franklin’s shot put and discus teams. Hampered by malnourishment, I saw a decline in my throwing distances of several feet from the year before. Within two months, I had lost more than 20 pounds.
Another response to the fear of weight gain is to deprive oneself of necessary nutrition. Contrary to the belief of many members of the public and medical professionals, “those in larger bodies are [often] not eating enough,” says Komine, “and in fact […] [they] could have very severe restrictive eating disorders.” One such eating disorder, anorexia, leads people to deprive themselves of caloric intake as they attempt to lose weight as quickly as possible. It has a higher mortality rate than any other mental health issue, according to the SCDMH. But even milder restrictive dieting provides little health benefit.
After my months of dieting, I decided to phase back into a looser system. I believed I had given myself the habits to maintain a lower body weight and eat healthy. But in restricting my diet so heavily, I had gained a false form of control. I returned to stress-eating within a few weeks, and eventually returned to the weight I’d started at. The shame that had driven me to restrict my eating was impatient. I felt that I needed to fit in as soon as possible, even if the diet was unhealthy.
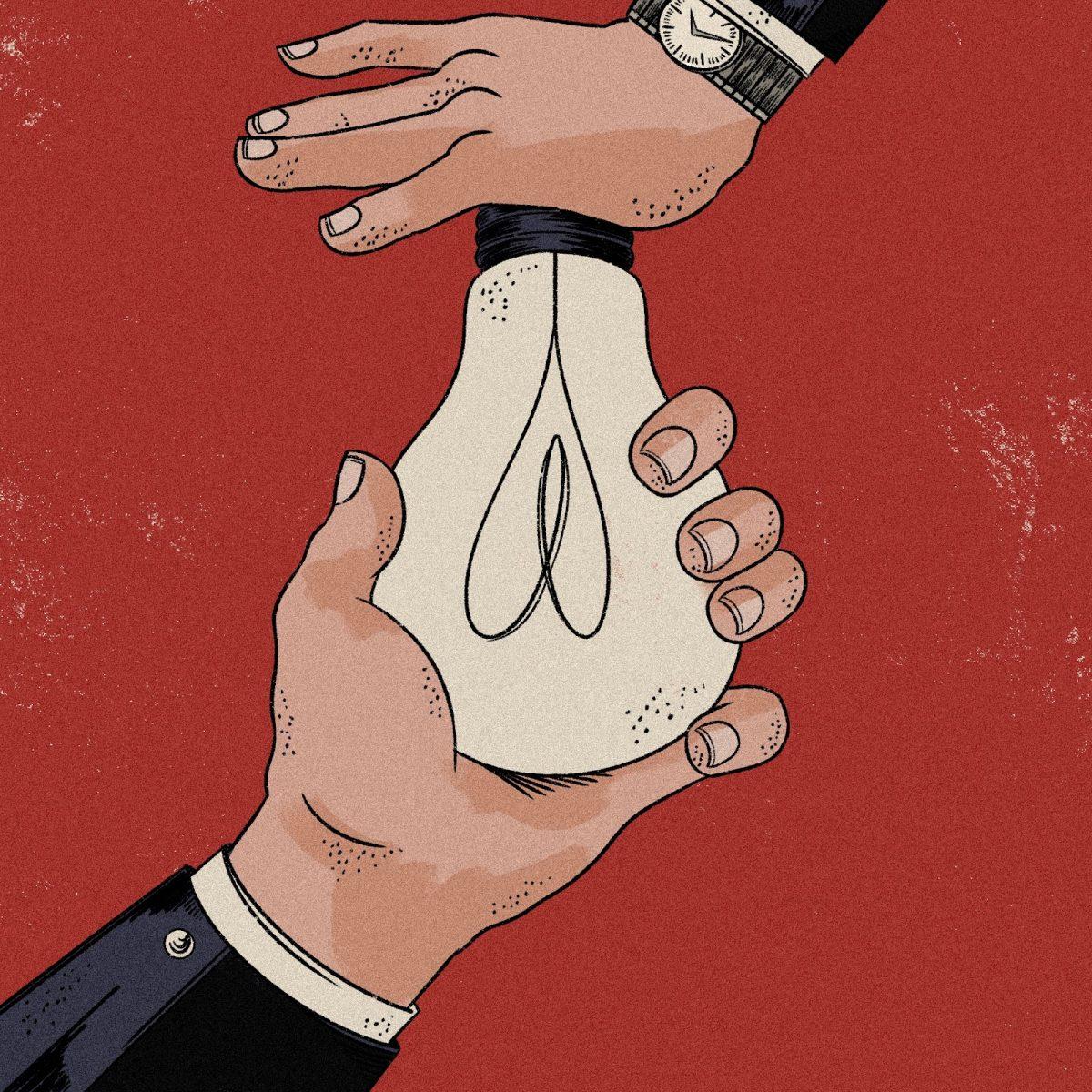
Komine refers to the pattern of heavy eating and dieting as a “binge-restrict cycle.” After periods of heavy dieting, people compensate with heavy binging. Komine says she “always tell[s her] clients [that binge-eating] is their body actually trying to take care of themselves, because we’re not designed to be in a place of starvation for very long.” Even what may seem like a successful weight-loss journey may be a phase in a long cycle of eating and starving.
It is true that there are some health risks associated with obesity. It is associated with other, more serious health issues, such as heart disease and diabetes. According to the CDC, medical costs for those with obesity were, on average, $1,861 higher than for those whose weight was classified as “healthy.” But helping people lose weight involves more than just telling them they weigh too much, and losing weight is not the same as staying healthy.
Weight is a limited tool for assessing health. Medical professionals often falsely attribute health issues to weight, dismissing accounts from the people describing their own problems. BMI was originally invented by mathematician Lambert Adolphe Jacques Quetelet, according to NPR, in order to assess obesity rates of white men on a population level, not to assess the health of individuals, according to Good Housekeeping. It was not applied to individuals until later. While it is associated with health risks like heart disease, obesity does not necessarily cause such health conditions, and chronic dieting is associated with heart disease as well, according to a study from the New England Journal of Medicine. And BMI measurements fail to account for the importance of mental health. Fat shaming has been linked with depression, according to a study by The Obesity Society, regardless of one’s actual BMI.
Fat shaming puts the burden on individuals without giving them the support to change their relationship with food. To better help people view food in a healthier way, Komine recommends the Intuitive Eating method. Intuitive Eating involves helping people enjoy eating and treating others with compassion regardless of their size. Unlike other nutritional plans, it is not a restrictive diet, as it promotes a more positive view of eating. It is a response to the rise of disordered eating that takes a more nuanced view of eating and health than older methods.
Fat shaming, even when well-intentioned, does not encourage healthy behaviors, and sometimes can have the opposite of the intended effect, leading people to gain weight as they cope with their shame by eating. It’s time to find an approach to nutrition that truly gets results, whatever Bill Maher may say.