Content warning: Mentions of sexual violence and medical abuse
“One [unique] thing about midwifery is that it comes from a place of believing that birth is normal,” says Laura Jenson, an assistant professor of clinical nursing at Oregon Health & Science University and a staff certified nurse midwife at Kaiser Permanente. She believes that, though midwifery is a part of the medical field, it differs from other medical professions due to the inherent belief that a person’s body is “made to birth their baby.” Midwifery isn’t about curing a particular injury or disease, but rather guiding the natural process of pregnancy and birth.
Chances are, if you’re reading this, someone gave birth to you. Pregnancy is a necessity for life, a biological function, and a deeply personal experience for each and every person who lives through it. The inherent challenges of pregnancy — hormonal changes, potential complications, and the birth itself — compounded with the unique and uncomfortable challenges pregnant people face in the U.S. make pregnancy a very complex experience to endure.
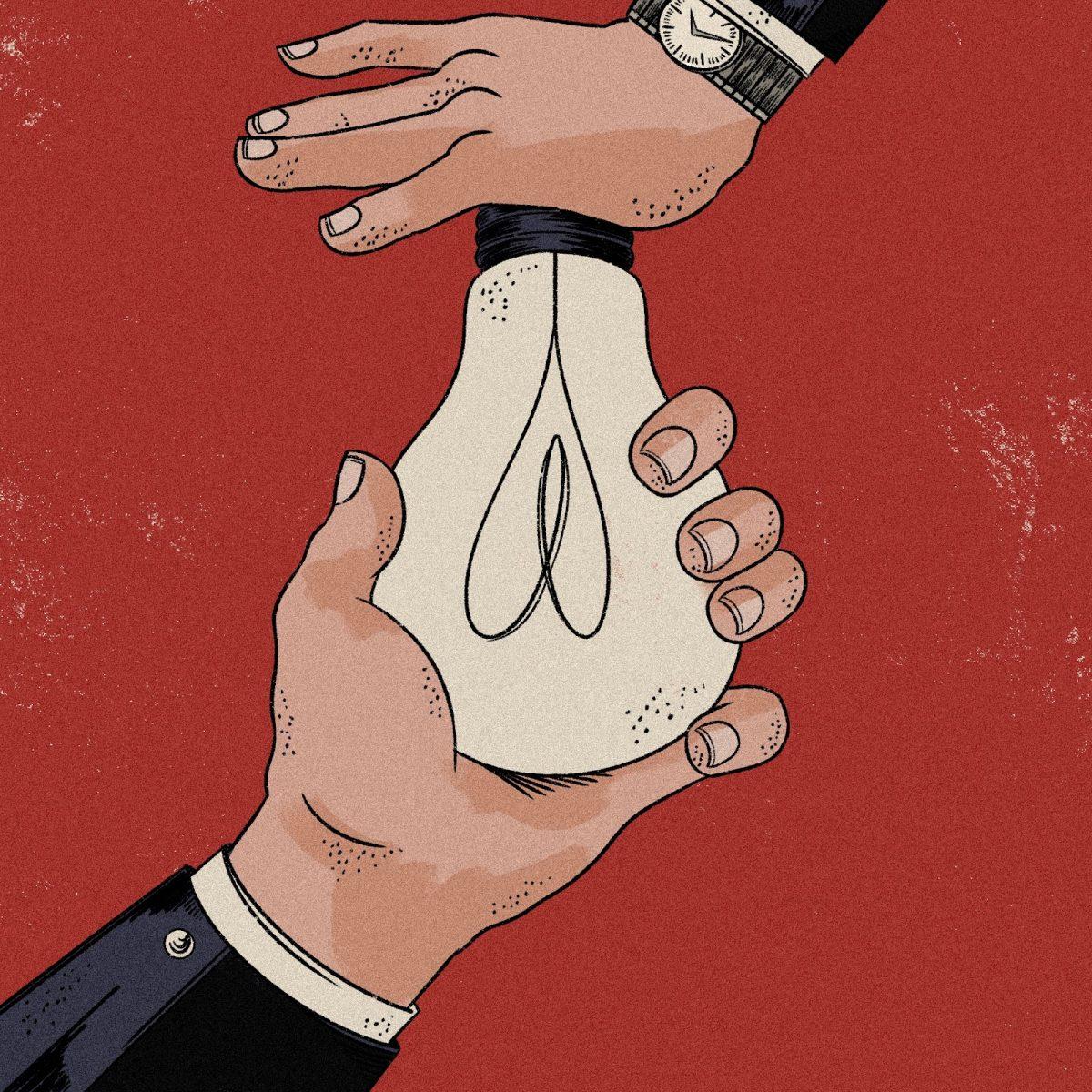
Before the colonization of North America, the care of pregnant people was in the hands of lay midwives — women, typically with no formal medical training, whose primary focus was the support and care of the pregnant person. These lay midwives differ from modern-day midwives, who are typically certified midwives or certified nurse midwives and have completed, at minimum, a graduate school education and a certification from the American Midwifery Certification Board.
The colonization of the Americas introduced European doctors and Western medicine to the continent. This may seem like a good thing — medical care is lifesaving, after all — but the reality is, many of the medical advancements in obstetrics we see today were on account of involuntary and often fatal testing on enslaved Black women.
Most notably, the modern cesarean section — also known as a “c-section” — was created by a slaveowner, François Marie Prevost, through repeated and forced experimentation on enslaved Black women. Along with these horrific experiments, European doctors started to criticize midwives, calling them incompetent and disparaging their work. As a result of these widespread anti-midwifery campaigns, the practice was systematically banned across the US over the course of the 20th century. Though midwives were eventually re-allowed into obstetrics, they had to fight for their education and certification, and are still fighting for certain privileges within the hospital hierarchy today. “That kind of [hierarchical] approach to healthcare is slowly being dismantled, but it’s still there,” says Jenson. “It’s reflected not just in [policy at individual hospitals] but also [in] the ways that laws are being made about people’s bodies. It’s very dystopian.”
Today, the U.S. has the highest maternal death rate of all high-income countries, at a rate of 22.3 deaths per 100,000 births. For a country with an $808 billion healthcare industry, these high death rates for an entirely natural and expectable aspect of human life are sobering. It’s impossible to separate this fact from the shunning of midwives from a space that they created.
The truth is, we will never understand the full extent of the damage that banning midwifery has inflicted on our nation. There are countless barriers that pregnant people face across the U.S. that are all, in some way, ripple effects of the anti-midwifery sentiment of the last century. Over 35% of all counties in the U.S. are considered “maternity care deserts” — places where there are no birthing facilities or obstetric clinicians. Even if people know exactly what they want from their pregnancy experience, they might not be able to get it since there are no facilities or practitioners to go to.
Luckily, in the Pacific Northwest, these maternity care deserts are very rare. Jenson considers obstetric care to be fairly reliable and accessible in Oregon, with maternity desert rates at a lower-than-average rate — 8.3% of counties. This standard of care is especially apparent when you compare Oregon to states like Texas, where almost half of all counties are maternity care deserts.
Birth, especially for the first time, is a scary thing. “You’re expected to do something that you’ve never experienced before, and … all of these expectations are put upon you about what kind of birth you should have, how you should act in birth, [and] should you do this or that,” says Jenson. She says her own pregnancy and birth were made easier by the fact that she’d delivered hundreds of babies before and was thus no stranger to pregnancy. But for many people, their first time giving birth is very stressful, with layers of confusion and uncertainty as to what is best for them or their baby.
Libby Borte, a Portland mother who’s given birth twice, says, “We do a big disservice [to pregnant people] by being a society dissociated from our bodies, and we have a lot of fear and disgust around our bodies.” Borte had an extremely positive experience with birth, both times delivering at home among a trusted group of midwives, family, and close friends. She describes giving birth as “the end of a race that you’ve chosen to run. You’re tired, and it kinda hurts, but it’s also like ‘You’re almost there!’”
In one way or another, birth is a part of everyone’s life — everyone must have been born, and many people will go on to give birth or have a loved one give birth. Obstetric care should be more accessible and widespread in the U.S. than it currently is, and overlooking the past wrongs that have occurred in this sector of the healthcare system won’t help us move on while maternal death rates stay high. We should try to focus on better practices, such as cultural sensitivity training and patient advocacy, that will help promote the well-being of all pregnant people in the U.S..