“We’re getting this money because people have died. It’s torn families apart. It’s changed the landscape in our country forever,” says Lisa Shields, the opioid settlement implementation manager for Oregon Health Authority (OHA). In the United States, settlements are currently being brought against many manufacturers and distributors of opioids for their role in deaths associated with the opioid crisis.
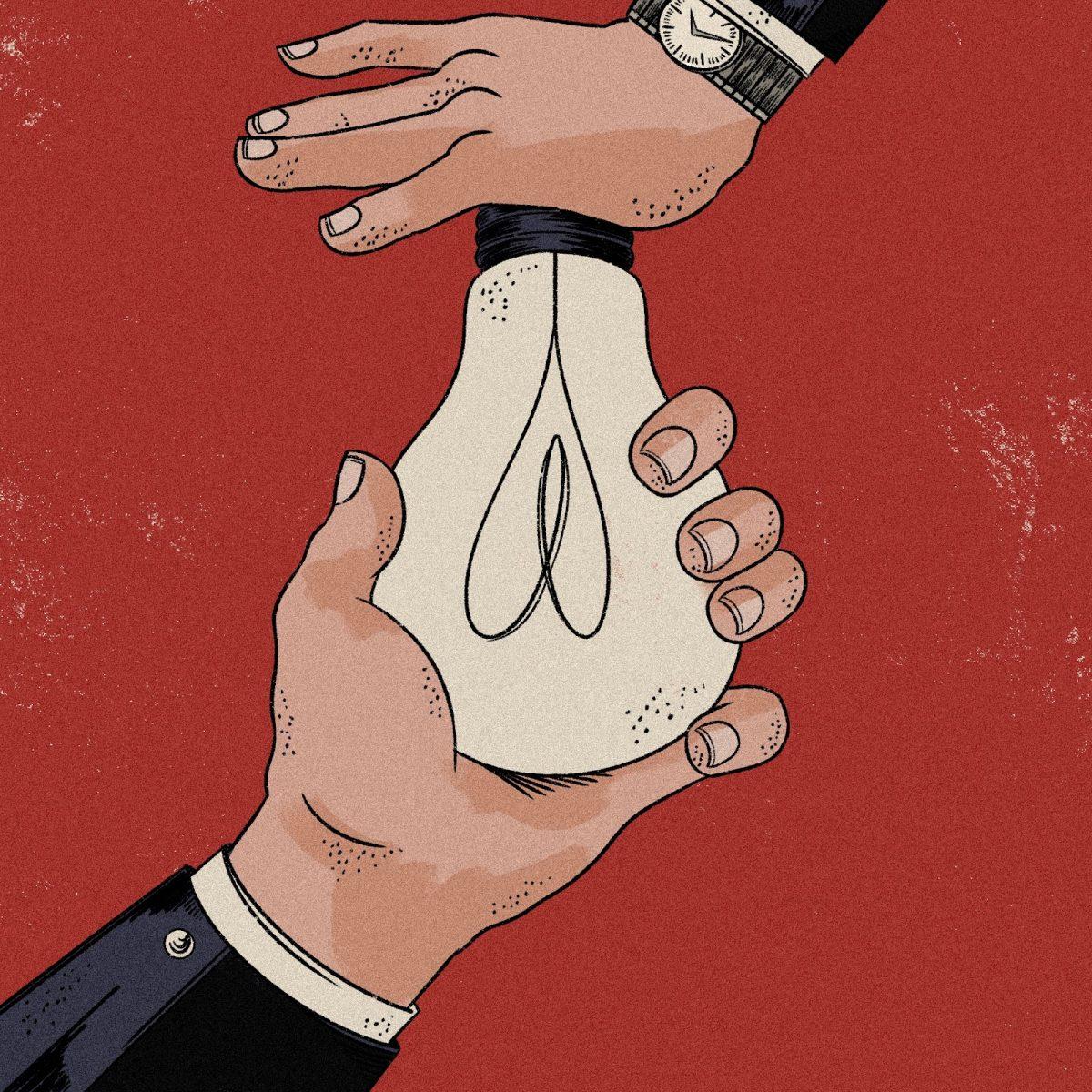
“Profit over people,” seems to be the unofficial mantra of large pharmaceutical companies. This prioritization is felt by many Americans; price gouging, among other symptoms of a diseased industry, means Americans routinely pay more for medications than they would in other countries. Recent settlements surrounding OxyContin serve, at the very least, as a reminder of these unethical tendencies.
Pharmaceutical companies use their large budgets to shamelessly market products — on television, online, and in print. Such advertising was restricted until 1997 when the US Food and Drug Administration (FDA) eased regulations, leading marketing focus to shift from doctors to consumers. Now, pharmaceutical companies spend over $6 billion on marketing directly to potential consumers; the average American sees nine of these ads each day.
This advertising can be deceptive. Federal law does not ban advertisements for prescription drugs, even ones that the FDA has determined may cause severe injury or addiction. Still, there are boundaries for medical advertising. The FDA requires that product claim ads — a common style of prescription drug ad that briefly introduces a drug to consumers — include the generic name of a drug, what condition it treats, and information about its benefits and risks. However, information the consumer needs about cost and safety can be left out, and companies can mislead their potential patients about the true effectiveness of a medication. These ads push narrative over information, getting people hooked on the bright-eyed, blue-sky, abundantly happy lives of the symptom-free people they portray.
To turn a pretty penny, pharmaceutical companies took to deception. A 2023 study led by researchers at the Johns Hopkins Bloomberg School of Public Health found that among top-selling prescription drugs, more money was spent promoting drugs with fewer added benefits to patients’ well-being than drugs with greater added benefits. The deception of consumers can go beyond overstating benefits or compensating for reality with cheery visuals — instead of being merely ineffective, prescription drugs can be actively harmful. In the case of Purdue Pharma and their prize drug OxyContin, their deceit contributed to the onset of the American opioid epidemic.
Purdue, a pharmaceutical company that develops, manufactures, and markets medications, was founded in 1892 but broke out of its chrysalis in 1952 when it was purchased by Arthur, Mortimer, and Raymond Sackler. Until recently, it was owned and managed by the Sacklers — one of America’s richest families, valued at $10.8 billion in 2020 according to Forbes. Purdue primarily manufactures pain medications with opioids like oxycodone, hydromorphone, and morphine.
It was in 1996, under the direction of the Sacklers, that Purdue prepared for the launch of their new wonder drug — OxyContin — a powerful opioid whose active ingredient is oxycodone. To convince medical professionals who were hesitant to prescribe strong opioids, Purdue aggressively marketed OxyContin as safe and effective. “Take the next step in pain relief,” reads an OxyContin ad, “When you know NSAIDs or acetaminophen will not be enough.”
Despite what Purdue promised prescribers, OxyContin was a highly addictive opioid. Initially marketed for chronic and cancer-caused pain, Purdue saw the opportunity to expand the reach of its “healing.” Internal Purdue documents disclosed in Kentucky legal proceedings revealed company executives eager to sell more, win over physicians’ prescription pads at dinner meetings, and avoid connotations of danger or addiction. Additionally, Purdue used national data compiled of prescribers to target those known to be heavy prescribers of opioids.
OxyContin’s distribution was widespread, and, when it hit an opioid-naive consumer base, mishandled. “[Pharmaceutical companies] were purposefully putting out opioids in enormous quantities out onto the market,” says lawyer Tom D’Amore, who represented nine Oregon counties in national opioid litigation. “They were pretty much acting like drug dealers, in that their drive for money was so strong that they were willing to risk the lives of our communities and our states.”
Purdue’s deceptive marketing to prescribers and glamorization to consumers ushered in the opioid epidemic. Since 1999, over 500,000 people in the U.S. have died due to opioid overdose, reports the Centers for Disease Control and Prevention. Continuing to market OxyContin as non-addictive throughout its promotional efforts, Purdue placed the blame of addiction on those who became addicted. Purdue instructed its pharmaceutical representatives to tell prescribers that only people with “addictive personalities” could become addicted to OxyContin, reports a 2022 paper published in the Journal of the Missouri State Medical Association.
By blaming consumers for becoming addicted, Purdue contributed to the public stigma around addiction that still exists today. “Reducing stigma is a real uphill battle,” comments Shields. “I’d say that [stigma is] probably our biggest barrier [to implementing settlement funds for programs addressing the opioid emergency] right now.”
In the decades of litigation to come, the Sacklers would deny personal wrongdoing. During a 2020 hearing, when asked if he would apologize for the role he played in the opioid crisis, former member of the Purdue board of directors David Sackler responded, “To the American people, I am deeply and profoundly sorry that OxyContin has played a role in any addiction and death. I believe I conducted myself legally and ethically.”
In a 2022 hearing anticipating the conclusion of a proposed settlement deal, David, Richard, and Theresa Sackler watched, via Zoom, two hours of testimonies by people who had lost loved ones to OxyContin. Throughout the testimonies the Sacklers sat quietly, and according to an NPR article published at the time, “[showed] no visible emotion or expression.”
In 2007, the company faced legal action in federal court for marketing OxyContin as less addictive than other pain medications, beginning its journey along the path of legal retribution. The opioid epidemic would not go quietly, quickly, or unnoticed, and someone — Purdue — needed to be held accountable. Purdue paid approximately $600 million in fines and penalties, and three of their executives paid $35 million.
More legal challenges were to come. In 2007, an additional $19.5 million went to 26 states and Washington D.C. over promoting “off-label” use; in 2015, they paid a $24 million settlement to Kentucky over misleading information about the drug; and in 2018, a $270 million settlement was reached with Oklahoma over deceptive marketing.
In September 2019, Purdue filed for bankruptcy in an attempt to resolve thousands of opioid lawsuits. The federal legal battle began. After two years of negotiations, a settlement was proposed in 2021 which would dissolve Purdue and see the Sacklers pay $4.5 billion — resolving 2,600 lawsuits and funding treatment programs nationwide. It also largely absolved the Sacklers of opioid-related liability — a contested term of the agreement. While the settlement was initially approved in bankruptcy court, it was objected to by a group of nine states — including Oregon — and the U.S. Trustee Program — the component of the Department of Justice responsible for overseeing bankruptcy cases. In June 2024, the U.S. Supreme Court rejected the plan, saying the bankruptcy of Purdue Pharma could not protect the Sacklers from lawsuits.
The Sacklers’ attempt to hide behind the Purdue bankruptcy settlement poses the ethical question of how accountability is properly handled when companies are targeted. Who made the marketing decisions? Who directed and fueled Purdue’s OxyContin frenzy? It wasn’t the company as an entity, it was corporate executives — human beings. “A lot of people wanted criminal charges against [the Sacklers],” comments D’Amore.
As of Jan. 23, 2025, a new $7.4 billion settlement has been agreed upon. It bars the Sacklers from selling opioids in the U.S., and requires them to give up ownership of the company and pay up to $6.5 billion over 15 years. $900 million is to be paid by Purdue. 15 state attorneys general, including Oregon’s, were involved in negotiating. The settlement does not provide any automatic immunity to the Sacklers. The funds from the settlement, which is in the final stages of negotiation, will directly contribute to opioid addiction treatment, prevention, and recovery programs across the nation, says Shields. Opioid settlement money is required to go to opioid treatment, prevention, and recovery uses.
“The opioid funding is really critical,” says Kristin Burke, a special project supervisor in Washington County’s Behavioral Health Division, who is currently involved with the county’s initiative to create the Center for Addictions Triage and Treatment (CATT). “If we hadn’t gotten the opioid dollars, we certainly would have had to scale back the size of the center or the scope of the services that are available.” Burke estimates that funding from opioid settlements is covering 15% of the project’s capital costs.
“We’ve been in an overdose crisis,” says Shields. OHA reports that in 2023, 1416 Oregonians died due to unintentional opioid overdose. Ten years ago overdoses were primarily from prescription drugs — now it’s fentanyl.
“We’ve certainly seen the impact of increased overdoses,” says Burke, adding that opioid overdoses have increased due to the current fentanyl epidemic. “It’s been pretty devastating to our community. … We really need to have additional support available to help people get off those substances.”
Burke emphasizes that “there’s no one size fits all to supporting community members struggling with opioid addiction.” Services must be available when people are ready and must be the right match for them — meaning additional treatment options need to be accessible within a community. “Funding things like Narcan and other services is just as important as creating centers like [the CATT]. We don’t feel the CATT is going to be an answer for everything,” she explains. “It’s part of an overall strategy and solution that is being deployed statewide.”
Even if opioid settlements cannot offer accountability, their impacts can be positive. “[For] a lot of these companies, the only thing that matters to them is money. And if lawsuits take away money from them, then that’s a good thing,” explains D’Amore. He recognizes that for billion-dollar pharmaceutical companies, the litigation chalks up to “just another expense on the income statement.” Pharmaceutical companies may just write off these lawsuits as the price of doing business. Still, he says, “There have been a lot of really wonderful things in terms of new treatment facilities and things that the cities, counties, and states have been able to do to fight this opioid epidemic.”
As the opioid epidemic changes — fentanyl and related synthetic opioids are now the main destructive drugs — the response must change with it. D’Amore says that the changing crisis is fueled by the “wheel of addiction,” explaining, “People would be addicted to opioids, and then when they couldn’t get opioids, they went to heroin. And when they couldn’t get heroin, they got into fentanyl.”
The CATT, Burke notes, is built to adapt to community needs. “It’s purposely designed to be very flexible. Say the need to respond to fentanyl decreases, but the need to respond to methamphetamine increases — we can change the treatment programming as needed to respond to our community.”
Still, funding is needed for these projects. Settlements pose a legally strenuous path to obtaining it, but may currently be the best option. To balance the moral scale, can’t we feel okay about taking money from these companies who have taken so much from communities? Doesn’t that feel like some form of progress? Perhaps these settlements shouldn’t be taken as “accountability” but as legal action required of the situation. Though the money may have positive impacts, it’s just “a drop in the ocean of the money [pharmaceutical companies] spent,” describes Shields.
“It doesn’t get us where we need to be,” says Shields. “[There are] so many gaps that this money can’t fill. There’s absolutely no way.” Opioid settlements are difficult — they try to seek retribution and accountability for the many lives lost in the past decades. In the labyrinthine tangle of past actions and current impacts, it can be hard to identify a true source of accountability. Burke reflects that sentiment, saying, “[Opioid settlement money] is certainly helpful, but it can only be a piece of the puzzle.”